Enfermedades de Glándula Mamaria

There is little cause for greater concern or alarm than finding a "lump" or tumor in the breast. You always think the worst and most dramatic. The reactions are different and very different, from people who consult the doctor quickly, to people who are afraid to tell anyone and therefore delay the diagnosis and possible solutions.
It is normal for a person to feel distressed and worried about presenting a "lump" in the breast, in principle the sooner you notice it and how small it is, the more chances of healing you will have if it is cancer. Not all "bultomas" are malignant, a professional should be consulted so that he can diagnose it correctly and if appropriate perform the appropriate treatment.
We cannot forget that breast cancer is the most frequent in women and is the second cause of mortality of women with cancer, after lung cancer but we must also note that if the tumor is small and there are no nodes the survival rate is greater than 95%. Mammography remains the test of choice.
- Overview and explorations
The mammary border or nipple line appears in the sixth week of embryo development and is identified in the form of an ectodermal thickening from the armpit to the groin. The caudal two-thirds of this line show regression and their abnormal persistence is often confused with nevi or moles. Aberrant breast tissue in the armpit or at any point outside the aforementioned border manifests itself during the hormonal stimulation of pregnancy and its treatment is surgical removal.
The decrease in the mother's estrogen levels after birth stimulates the production of prolactin by the newborn with colostrum (witch's milk) secretion for several days in boys and girls.
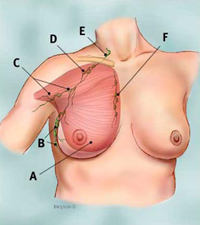
Except for mild hypertrophy during the neonatal period and puberty, the male breast area shows little change throughout life. The prepubertal "mound" of the woman arises between the ages of 11 and 15. There is lobe formation after the first ovulation. The sinus of the young adult extends from the second to the sixth ribs and from the sternum to the anterior axillary line. E1 glandular tissue has a circular shape, except for Spence's tail, which reaches the armpit. Cooper's fibrous ligaments suspend glandular tissue from the anterior superficial aponeurosis under the skin. The subareolar area and nipple contain smooth muscle that contracts with tactile stimulation.
The lymph nodes in the area of the inner and axillary mammary are responsible for the drainage of the breast.
Axillary levels: I, outside the pectoralis minor; II, below the pectoralis minor; III, inside the pectoralis minor. The Rotter ganglia constitute a group that is located between the pectoralis major and minor muscles. Drainage is done from the bottom up and eventually to supraclavicular ganglia, and then through the thoracic duct to the venous system. The average number of lymph nodes recorded in operations is five internal mammary nodes and 20 axillary nodes (levels I, II and III).
Physiology
The development and function of the breast is initiated by various hormones. Estrogen is known to stimulate the formation of the mammary ducts. Progesterone begins the development of breast lobules and the differentiation of epithelial cells. Prolactin stimulates lactogenesis. Cyclic changes: the volume increases almost 50% after the eighth day of the menstrual cycle. Vascular congestion and lobular proliferation show regression with menstruation.
- Pregnancy and lactation: the lobular alveolar ducts proliferate after the regression that occurs when the breastfeeding phase ceases. The nipple and areola are darkened and the Montgomery glands of the areola protrude. Appears nestries.
- Menopause: the lobules involute and fat replaces the parenchyma.
- Aberrations: Asymmetrical development or virginal hypertrophy in young girls can be surgically corrected after maturity. Gynecomastia in pubertal males is corrected if there is no reversal or hormonal abnormalities.
Physical examination
- Inspection: The operator can more easily detect asymmetry, skin depressions, edema and nipple inversion if the woman is seated, with her hands on the hip and then raises them above the head.
- Palpation: With the patient seated and then erect, the operator explores the supraclavicular area and axillary fossa, and also Spence's tail and central breast tissue. The entire breast is checked again with the woman lying on her back and with her arms above her head. Important features of a tumor or node are its size, shape, mobility, and fixation.
- Studies:
- Mammography: The American Cancer Society recommends "basal" mammograms between ages 35 and 40, then every two years between ages 40 and 50, and every year after age 50. If there is a family history, the first mammogram must be obtained at age 35 and an annual plaque after age 40. The mammogram assesses stromal changes, in contrast to the fatty areas of the breast, so it is more accurate in the fatty breasts of postmenopausal than in the glandular sinuses of premenopausal breasts. Suspicious patterns of carcinoma include skin thickening, stromal densities with "radiated" invasion of the parenchyma, and microcalcifications (debris expelled into the ducts by rapidly dividing cells, especially common in intracanalicular cancers). Mammography is especially useful in the exploration of non-palpable lesions, to study the contralateral sinus in women with cancer, and in the follow-up of the ipsolateral breast after a conservative treatment of Cancer. The frequency of false positive results is 11% and that of false negatives 6%. Prospective studies demonstrated earlier detection of cancer and improved survival through mammography identification. Xeroradiography is similar to mammography but positive rather than negative images and increases radiation exposure, which is why it is not recommended. Thermography: tumors or infections generate "hot spots", but they are an unreliable method.
- Ultrasonography: cysts are distinguished from solid lesions by ultrasound, but with this method microcalcifications are not detected. Needle aspiration is a simpler and less expensive technique for detecting cysts. Its main indication is to study suspicious lesions not palpable in mammography.
- Other methods: Computer tomography and nuclear magnetic resonance imaging are still in the experimental phase in the detection of breast cancer.
- Ductography: consists of the injection of radiopaque contrast into a milk duct. It is indicated by nipple secretions, particularly if they are bloody.
- Benign breast pathology
Fibrocystic mastopathy
Called in many ways, among other chronic cystic mastitis, this disorder increases in incidence with age, but tends to generate more symptoms in young women, and before menstruation pain and swelling of the breasts are also noticed. Only women with severe hyperplasia or atypia on biopsy are at increased risk of carcinoma. Claims of symptomatic relief with vitamin E ingestion or withdrawal from caffeine or xanthine derivatives have never been substantiated.
They have been used effectively in the treatment Danazol (synthetic androgenic analogue), tamoxifen (an antiestrogen) and even progesterone.
Cysts
These circumscribed, firm, round masses range from 1 mm to several centimeters in diameter and can increase in size at the end of the menstrual cycle. In aspiration, in typical form, the fluid is clear or brownish green and does not require cytological examination. Biopsy is indicated if the fluid is bloody, if the mass does not show complete resolution after aspiration, or if the mentioned fluid accumulates.
Fibroadenomas
These lobular, firm, leathery and circumscribed masses are usually solitary and appear in young women; They are best treated by ablation in women older than 25 years. In younger patients, needle aspiration cytology studies should be limited and kept under surveillance.
Papiloma canalicular
On average, 33% of women with bloody nipple discharge have intracanalicular papilloma, even though nearly 20% have carcinoma. The diagnosis is confirmed by ductography. Ablation of the main duct system and breast tissue in the subareolar area is practiced with the help of a tear tube as a guide, which is introduced into the duct it secretes.
Other injuries
- Sclerosing adenosis: irregular fibrotic areas of breast tissue with microcalcifications, which need biopsy to differentiate from carcinoma.
- Fat necrosis: on average, only 50% of women with fat necrosis remember the trauma related to it, which causes areas of interstitial fibrosis, firm and irregular with skin retraction often confused with carcinoma, until the histopathological study Myoblastoma of granulosa cells of the breast, of macroscopic appearance similar to incipient breast cancer.
- Mondor's disease, which is thrombophlebitis of a superficial vein of the breast, often with pain and skin retraction.
- Acute infections are more common in breastfeeding women who suffer nipple abrasions, and are often accompanied by pain and erythema. Cellulitis can be treated with antibiotics, but abscesses require incision, cutting of loculations, and declining drainage (usually identified in Staphylococcus aureus culture). Women who do not breastfeed need biopsy and drainage to differentiate between duct ectasia and abscesses that are secondary to the obstruction caused by canalicular carcinoma.
- Chronic infection is rare, except in immunosuppressed patients, but histologically it is usually caused by tuberculosis, which comes from the lungs or from erosion of a costal cartilage by a mediastinal node.
Mammary Gland Diseases: Carcicoma
Breast carcinoma is the most common cancer in women in the United States, and since 1940 the age-adjusted incidence has increased; It is currently diagnosed in one in nine Americans during their lifetime. The death rate from breast cancer is second only to lung cancer.
Its cause is likely to be multifactorial. Female sex is a predisposing factor, since only one male shows breast carcinoma for every 100 women diagnosed.
The incidence increases with age. It begins after age 20 and reaches a stable level (plateau) around menopause, then increases net after that change. Genetic factors are important in 15% of cases, and are most noticeable in women whose mother had carcinoma in both breasts before menopause. England and Wales have the highest national breast cancer mortality and Japan the lowest.
The highest risk is related to nulliparity and the first pregnancy in the last years of fertility. Estrogens induce breast cancer in mice, but no theory of induction by hormones or birth control pills has been substantiated in humans.
Among the risk factors that have been proposed are obesity, abundant consumption of animal fats and viral factors transmitted by breast milk.
The natural course of the disease has been cited in studies since the end of the last century, at Middlesex Hospital, London, in which the median survival in 250 untreated women was 2.7 years; Survival was calculated based on the description of the onset of the first symptoms.
The five-year survival was 18% and the decennial 3.76%. Necropsies showed that 95% of women died of breast carcinoma and of them 75% had breast ulcers. Biological features of breast cancer: typical scirrhosal adenocarcinoma begins in the superoexternal quadrant (45%) of the left breast (60%) and it takes 30 duplications from the single-cell stage, for a period of five to eight years to reach a palpable size (1 cm in diameter).
Metastases arise when the tumor is 0.5 cm in diameter and the prognosis is adversely influenced by the number of axillary lymph nodes affected. With the aforementioned enlargement fibrosis shortens the Cooper's ligament and there is the characteristic depression or dimpling of the skin.
Systemic spread is most common to lungs (65%), bone (56%), and liver (56%).
The diagnostic investigation should be done in an orderly manner. In any suspicious lesion, aspiration biopsy should be performed and then by partial (incisional) removal, in the direction of the skin folds (periareolar), or as a convenient resource in case of possible segmental resection or subsequent mastectomy. Staging can be done before definitive treatment and includes a chest x-ray and liver function tests. Skeletal x-rays and bone scans are not required when there are no specific symptoms.
- Self-review
Steps to follow
 Lying
Lying- Put your arms on both sides
- Check your breasts for nodules, retractions, irregular shapes, or other changes
- Repeat the procedure with your arms above your head.
- Now with his hands on his hips and chest muscles tense.
- Finally, bend over and watch your breasts once more for any changes.
- Lie on your back in a comfortable position and place a pillow under your left shoulder.
- Examine your entire left breast with your right hand, following each of the figures shown below.
- Place your fingers flat against the breast tissue, pressing lightly, medium and firmly making small and larger circles.
- Now move the pillow to your right shoulder and examine your entire right breast

In the shower
 Check your breasts and armpits for any lumps or thickening.
Check your breasts and armpits for any lumps or thickening.- Examine your breasts in the shower using the same procedure you used in the previous step.
- Your soapy hands will slide more easily over wet skin.
Notes
- It is recommended not to perform this self-examination in premenstrual season.
- If you notice any nipple discharge during these procedures, or at any time, tell your doctor.